Aim: Dynamic assessment of trends over time in patient- and transplant-specific characteristics and outcomes for patients undergoing 1st allogeneic haematopoietic cell transplant (allo-HCT) for Myelofibrosis (MF).
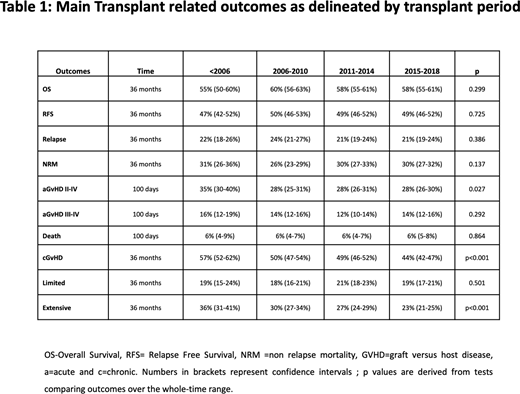
Methods and Results: A total of 4142 MF patients were analysed who underwent allo-HCT between 1995-2018 (24-year period) across 278 centres based on data reported to the European Society for Blood and Marrow Transplantation. For analysis, 4 cohorts were considered based on year of allo-HCT: <2006 n=389 (9.4%), 2006-2010 n=910 (22%), 2011-2014 n=1148 (27.7%) and 2015-2018 n=1695 (40.9%). A steady increase in MF allo-HCT activity over time was apparent paralleled with increasing numbers of participating transplant centres. A total of 2603 (62.8%) patients were male, 3239 (78.2%) had Primary MF, 409 (9.9%) and 494 (11.9%) post-Polycythaemia Vera and post-Essential Thrombocythaemia MF, respectively. An increased median interval (lnterquartile range (IQR)) between diagnosis and transplant was evident over time (<2006 median 20.8 (8.9-62.2) months versus 36.2 (11.6-107.5) months in 2015-2018 period;p<0.001), potentially reflecting increased availability of therapeutics in recent eras (untreated patients <2006= 59.4% versus 2015-2018=23.7%). Median recipient age (IQR) increased over time by ~ a decade between earliest cohort and most recent: <2006, 49.4 years (43.1-55.3) versus 59.3 years (53.4-64.8)2015-2018. Prior to 2006, patients >60 years accounted for 8.7% of adults undergoing allo-HCT whereas for 2015-2018 this was 47%. Over time, increasing number of patients with a Karnofsky performance status (KPS) <90 underwent allo-HCT (<2006=19.7% versus 36.1% 2015-18; p<0.001). Peripheral Blood (PB) was the predominant stem cell source and utilisation increased over time, accounting for 74.8% <2006 and 92.2% within 2015-2018 cohort. Cord blood utilisation was limited to <1% throughout the 24-year study period. Significant shifts towards use of unrelated donors (URD) in more recent periods was apparent (p<0.001). Moreover, increased use of mismatched related donors (MMRD) was particularly evident in 2015-2018 cohort; n=152 (9%) versus n=74 (3%) cumulative for other 3 cohorts combined; p<0.001. Decreased use of myeloablative and TBI- based conditioning was evident over time (p<0.001). Specifically, there was increased use of busulphan-based regimens (<2006: 44.2% versus 2015-2018: 72%). Regarding T cell depletion, trends demonstrated increased use of anti-thymocyte globulin (ATG) over time (<2006=37.3% vs 69.9% 2015-2018; p<0.001). Median time to both neutrophil (median 18 days across all cohorts) and platelet engraftment was similar in all 4 cohorts, with no significant variation when stratified by period of transplantation. Allo-HCT outcomes, survival, GVHD and relapse endpoints are shown for all 4 cohorts in Table 1. Overall for the entire group, significant factors associated with worse OS, RFS and NRM remained older age and a poor KPS (<90). No significant differences between cohorts were noted for either estimated 3-year OS (<2006=55% (50-60%), 2006-2010=60% (56-63%), 2011-2014 and 2015-2018= 58% (55-61%); p=0.299) or non-relapse mortality (NRM (Table 1); p=0.523), despite increasing numbers of older, less fit patients, and more frequent HLA-mismatched transplants over time. To investigate survival findings in more detail an adjusted model will be presented including period of allo-HCT and transplant-related variables. Cumulative incidence of relapse at 3 years was similar across all cohorts, suggesting no significant changes with time. Most common causes of death across all 4 cohorts remained GVHD and infection. Of note, rates of acute (a)GVHD grade II-IV by day +100 decreased from the earliest cohort <2006 compared to the later groups (p=0.027) as did rates of overall chronic (c) GVHD whereby this was evident in 57% (95% CI 52-62%) <2006 cohort compared to 44% (95% CI 42-47%) in the 2015-2018 group, predominantly reflected by reductions in extensive cGVHD (Table 1).
Conclusions: Despite a marked increase over this 24-year period in recipient age, RIC regimen utilisation and use of both URD and MMRD, this comprehensive analysis demonstrates stable OS and EFS rates. However, rates of GVHD have decreased over time, in particular extensive cGVHD. Further work is required to improve both the considerable NRM and relapse rates which remain significant.
McLornan:JAZZ PHARMA: Honoraria, Speakers Bureau; CELGENE: Honoraria, Speakers Bureau; NOVARTIS: Honoraria, Speakers Bureau. Platzbecker:Amgen: Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Geron: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding. Chevallier:Incyte Corporation: Honoraria. Martínez-Lopez:Altum, Hosea: Membership on an entity's Board of Directors or advisory committees, Patents & Royalties; Vivia Biotech: Honoraria; Amgen: Speakers Bureau; Takeda: Speakers Bureau; Roche: Speakers Bureau; Janssen: Speakers Bureau; Incyte: Research Funding, Speakers Bureau; Bristol Myers Squibb: Research Funding, Speakers Bureau; Novartis: Research Funding. Yakoub-Agha:Celgene: Honoraria; Jazz Pharmaceuticals: Honoraria; Novartis: Honoraria; Gilead/Kite: Honoraria, Other: travel support; Janssen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal